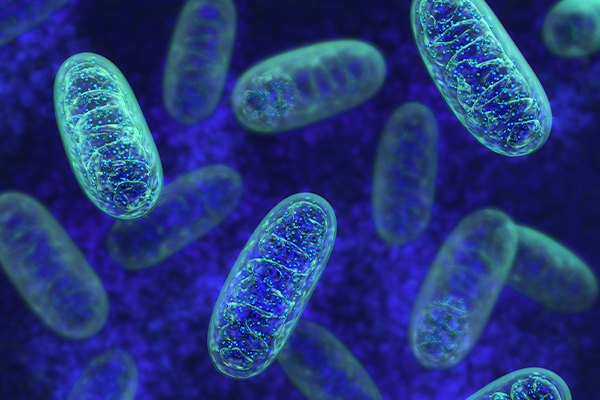
Mitochondria are often called the powerhouses of the cell, and for good reason. These tiny organelles convert nutrients into adenosine triphosphate (ATP), the energy currency that powers nearly every cellular process. Without properly functioning mitochondria, cells struggle to perform their essential tasks, leading to widespread physiological consequences.
Mitochondria use a process called oxidative phosphorylation to generate ATP. This involves breaking down carbohydrates, fats, and proteins, utilizing oxygen to create energy efficiently. Any disruption in this process can lead to an energy deficit, impairing vital bodily functions and increasing susceptibility to chronic diseases.
Beyond energy production, mitochondria play crucial roles in cellular signaling, calcium storage, and apoptosis (programmed cell death). They help regulate immune responses, influence gene expression, and even participate in hormone synthesis. Dysfunction in these areas can contribute to a wide range of health issues, from neurodegenerative diseases to metabolic disorders.
Healthy mitochondria are essential for maintaining cellular homeostasis. They assist in detoxifying harmful free radicals, reducing oxidative stress, and keeping inflammation in check. When mitochondrial function declines, cells become vulnerable to damage, accelerating aging and chronic disease development.
What is Mitochondrial Dysfunction?
Fails
Mitochondrial dysfunction occurs when these organelles fail to generate sufficient ATP, leading to cellular energy deficits. This can result from genetic mutations, environmental stressors, or a combination of factors that impair their efficiency.
Several factors contribute to mitochondrial dysfunction, including poor diet, chronic stress, exposure to environmental toxins, infections, and genetic predispositions. Nutrient deficiencies, particularly in coenzymes like NAD+ and CoQ10, also play a significant role in declining mitochondrial health.
When mitochondria become compromised, the ripple effect is widespread. Energy-intensive organs like the brain, heart, and muscles are especially vulnerable. This can manifest as cognitive decline, cardiovascular problems, and chronic fatigue.
Excessive oxidative stress results from an imbalance between free radicals and antioxidants. Damaged mitochondria generate more free radicals, exacerbating oxidative stress and further impairing mitochondrial function—a vicious cycle that accelerates chronic illness.
Exposure to heavy metals, pesticides, air pollution, and endocrine-disrupting chemicals can impair mitochondrial function. These toxins interfere with the electron transport chain, disrupt cellular signaling, and contribute to inflammation and disease progression.
How Mitochondrial Dysfunction Leads to Chronic Illness
A deficiency in ATP means cells cannot maintain optimal function. This impacts tissue repair, immune defense, and even neurological processing, making the body more susceptible to chronic illnesses.
Chronic inflammation damages mitochondria, and in turn, malfunctioning mitochondria perpetuate inflammation. This cycle is linked to autoimmune disorders, cardiovascular disease, and metabolic dysfunctions.
Mitochondria influence immune system regulation. When dysfunctional, they can trigger inappropriate immune responses, leading to conditions like lupus, rheumatoid arthritis, and multiple sclerosis.
The Connection Between Mitochondrial Dysfunction and Neurological Diseases
Brain cells are heavily reliant on mitochondrial energy. Dysfunction contributes to neurodegenerative conditions such as Alzheimer’s, Parkinson’s, and multiple sclerosis, impairing cognitive function and motor control.
Hormone-producing glands require significant energy to function. Mitochondrial dysfunction can lead to thyroid disorders, adrenal fatigue, and insulin resistance, disrupting the endocrine system.
Mitochondria regulate metabolism and energy expenditure. Dysfunction is associated with insulin resistance, weight gain, and metabolic syndrome, making it a key factor in diabetes and obesity.
Recognizing the Symptoms of Mitochondrial Dysfunction
Below are the common symptoms of mitochondrial dysfunction:
- Chronic fatigue. This is a hallmark symptom, as energy production is compromised. This can be misdiagnosed as depression, thyroid disorders, or chronic fatigue syndrome.
- Brain Fog and Cognitive Decline. Difficulty concentrating, memory lapses, and mental fatigue may stem from reduced ATP availability in brain cells, affecting neurotransmitter production and cognitive processing.
- Muscle Weakness and Chronic Pain. Insufficient ATP leads to muscle dysfunction, cramping, and pain. Fibromyalgia and other chronic pain conditions often have mitochondrial dysfunction as an underlying factor.
- Digestive Issues and Mitochondrial Malfunction. Mitochondria support gut lining integrity and digestive enzyme production. Dysfunction can result in bloating, food intolerances, and irritable bowel syndrome (IBS).
Why Mitochondrial Dysfunction Can Cause Mood Disorders and Anxiety
Mitochondrial health affects neurotransmitter balance. Dysfunction has been linked to anxiety, depression, and mood instability, often due to impaired serotonin and dopamine production.
Symptoms are often vague and overlap with other conditions, making diagnosis challenging. Conventional medicine frequently overlooks mitochondrial function in chronic disease assessment.
Lactate and pyruvate ratio tests, muscle biopsies, genetic testing, and metabolic assessments can help identify mitochondrial dysfunction.
Many diagnostic tools focus on end-stage disease rather than early dysfunction. Functional medicine approaches offer more nuanced testing to detect early mitochondrial decline.
Healing and Supporting Mitochondrial Health
To boost mitochondrial health and avoid dysfunction, below are steps that can be taken:
- Boosting nutrition. A diet rich in antioxidants, healthy fats, and micronutrients can enhance mitochondrial efficiency and repair.
- Taking Supplements. CoQ10, PQQ, NAD+, alpha-lipoic acid, and magnesium support mitochondrial regeneration and energy production.
- Exercising. Aerobic exercise and strength training stimulate new mitochondrial growth, improving overall function and resilience.
- Getting enough sleep. Deep sleep promotes mitochondrial maintenance, detoxification, and energy restoration.
Detoxification and Mitochondrial Health
Effective detoxification supports mitochondrial health by reducing the accumulation of harmful substances. The liver, kidneys, lymphatic system, and gut play key roles in eliminating toxins, but they require proper nutritional and lifestyle support. Consuming antioxidant-rich foods such as leafy greens, cruciferous vegetables, and berries can help neutralize free radicals, while sulfur-containing foods like garlic and onions enhance liver detoxification. Hydration, regular exercise, and infrared sauna therapy further promote the removal of toxins.
Supporting mitochondrial function also involves reducing exposure to harmful chemicals in personal care products, plastics, and pesticides. Additionally, supplements like glutathione, alpha-lipoic acid, and CoQ10 aid in cellular repair and energy metabolism. By prioritizing detoxification, individuals can optimize mitochondrial function, enhance energy levels, and support long-term health and vitality.




